Heart failure, also known as congestive heart failure, is a chronic condition where the heart is unable to pump blood efficiently to meet the body’s demands. Over time, this decreased pumping ability can lead to damage of organs and fluid buildup in the lungs. The initial treatment approach involves incorporating lifestyle changes such as exercise and taking prescribed medications. In severe cases, surgery may be necessary to help improve the heart’s function. The prognosis of an individual with heart failure varies and is influenced by a number of factors, including the person’s overall health, the severity of their condition, and their ability to follow a self-care plan.
How common is heart failure?
Approximately 0.26%-0.8% people will be diagnosed with Heart Failure every year it about 7,000 Georgian citizens. (According to word statistics)
Heart failure, also known as congestive heart failure, is a major reason for hospitalization among individuals over 65 years of age.
Heart failure types
There are many causes of heart failure, but the condition is generally broken down into these types:
Left-sided heart failure.
Heart failure with reduced left ventricular function (HF-rEF)
The left ventricle, located in the lower left chamber of the heart, expand and loses its ability to contract strongly enough to circulate an adequate amount of oxygen-rich blood throughout the body.
Heart failure with preserved left ventricular function (HF-pEF)
The ventricles in the lower chambers of the heart are abnormally thick and rigid, preventing proper relaxation and full filling. As a result, each contraction of the heart pumps a reduced amount of blood to the body. Despite this, the heart’s contraction and pumping remain normal.
Right-sided heart failure
Heart failure can impact the right side of the heart, with left-sided heart failure being the most prevalent cause. Other factors that contribute include lung conditions and issues with other organs.
Congestive heart failure
This is a state in which your heart hasn’t been able to handle the blood volume. This causes an accumulation in other parts of your body, most commonly in your lungs and lower extremities (feet/legs).
Heart failure complications
Some of the complications from heart failure include:
- Irregular heartbeat.
- Sudden cardiac arrest.
- Heart valve problems.
- A collection of fluid in your lungs.
- Pulmonary hypertension.
- Kidney damage.
- Liver damage.
- Malnutrition
Heart failure stages
Stage A
In Stage A, individuals are categorized as being at high risk for heart failure, also known as pre-heart failure. This designation is given to those with a family history or who have one or more of the following medical conditions: hypertension, diabetes, coronary artery disease, metabolic syndrome, a history of alcohol abuse, rheumatic fever, a family history of cardiomyopathy, or a history of using heart-damaging drugs such as certain cancer medications.
Stage B
Stage B, referred to as pre-heart failure, is when a healthcare provider has diagnosed systolic left ventricular dysfunction but the individual has yet to exhibit symptoms of heart failure. A common diagnostic tool in Stage B is an echocardiogram (echo) revealing an ejection fraction (EF) of 40% or lower. This stage encompasses individuals with heart failure and reduced EF (HF-rEF) caused by any factor.
Stage C
People with Stage C heart failure have a heart failure diagnosis and currently have or previously had signs and symptoms of the condition.
There are many possible symptoms of heart failure. The most common are:
- Shortness of breath.
- Feeling tired (fatigue).
- Less able to exercise.
- Weak legs.
- Waking up to urinate.
- Swollen feet, ankles, lower legs and abdomen (edema).
Stage D and reduced EF
Individuals in Stage D of HF-rEF experience severe, persistent symptoms despite treatment efforts. This is the final stage of heart failure.
Symptoms of heart failure
Symptoms of heart failure include:
- Shortness of breath.
- Feeling tired (fatigue) and having leg weakness when you’re active.
- Swelling in your ankles, legs and abdomen.
- Weight gain.
- Need to urinate while resting at night.
- Rapid or irregular heartbeats (palpitations).
- A dry, hacking cough.
- A full (bloated) or hard stomach, loss of appetite or upset stomach (nausea).
There may be times that your symptoms are mild or you may not have any symptoms at all. This doesn’t mean you no longer have heart failure.
Unfortunately, heart failure usually gets worse over time. It’s important to let your doctor know if you have new symptoms or if your symptoms get worse.
Heart failure (congestive heart failure) causes
The likelihood of developing heart failure increases with age, even though the risk of heart failure itself remains constant. Heart failure can also be caused by several medical conditions that affect the heart muscle. Common conditions include:
- Coronary artery disease.
- Heart attack.
- Heart issues present at birth (congenital heart disease).
- High blood pressure (hypertension).
- Arrhythmia (abnormal heart rhythms, including atrial fibrillation).
- Kidney disease.
- Having obesity.
- Tobacco and recreational drug use.
- Some drugs used to fight cancer (chemotherapy) can lead to heart failure.
Heart Failure Diagnosis
In order to determine if you have heart failure, your healthcare provider needs to know about your symptoms and medical history. They will ask you about things such as:
- Other health conditions you have, such as diabetes, kidney disease, chest pain (angina), high blood pressure, high cholesterol, coronary artery disease, or other heart problems.
- If you have a family history of heart disease or sudden death.
- If you smoke or use tobacco.
- How much alcohol you drink.
- If you’ve had chemotherapy and/or radiation.
- The medications you take.
You’ll also have a physical exam. Your provider will look for signs of congestive heart failure and diseases that may have caused your heart muscle to become weak or stiff.
The importance of ejection fraction
Your ejection fraction (EF) is one way to measure the severity of your condition. If it’s below normal, it can mean that you have heart failure. Your ejection fraction tells your healthcare provider how good of a job your left or right ventricle is doing at pumping blood.
Several non-invasive tests can measure your EF. With this information, your healthcare provider can decide how to treat you or find out if a treatment is working as it should.
A healthy left ventricular ejection fraction (LVEF) ranges from 53% to 70%. For example, an LVEF of 65% indicates that 65% of the blood in the left ventricle is expelled with each heartbeat. The EF can fluctuate based on the heart’s condition and the effectiveness of treatment.
Types of tests to diagnose heart failure.
You’ll have tests to see how bad your heart failure is and what caused it. Common tests include:
- Blood tests.
- NT-pro B-type Natriuretic Peptide (BNP) blood test.
- Cardiac Catheterization.
- Chest X-ray.
- Echocardiogram (echo).
- Magnetic resonance imaging (MRI).
- Electrocardiogram (EKG or ECG).
- Multi-gated Acquisition Scan (MUGA scan).
- Stress test.
Heart failure treatments
Your treatment will depend on the type of heart failure you have and, in part, what caused it. Medications and lifestyle behaviors are part of every treatment plan. Your healthcare provider will talk to you about the best treatment plan for you. Treatment is the same, regardless of gender.
As heart failure gets worse, your heart muscle pumps less blood to your organs, and you move toward the next stage of heart failure. Since you can’t move backward through the heart failure stages, the goal of treatment is to keep you from moving forward through the stages or to slow down the progression of your heart failure.
Stage A treatment
The standard treatment regimen for Stage A heart failure patients encompasses:
- Regular exercise, being active, walking every day.
- Stopping the use of tobacco products.
- Treatment for high blood pressure (medication, low-sodium diet, active lifestyle).
- Treatment for high cholesterol.
- Not drinking alcohol or using recreational drugs.
- Angiotensin-converting enzyme inhibitor (ACE-I) or an angiotensin II receptor blocker (ARB) if you have coronary artery disease, diabetes, high blood pressure, or other vascular or cardiac conditions.
- Beta-blocker if you have high blood pressure.
Stage B treatment
The usual treatment for people with Stage B heart failure my include:
- Treatments listed in Stage A.
- Angiotensin-converting enzyme inhibitor (ACE-I) or angiotensin II receptor blocker (ARB) (if you aren’t already taking one).
- Beta-blocker if you’ve had a heart attack and your EF is 40% or lower (if you aren’t already taking one).
- Aldosterone antagonist if you’ve had a heart attack or if you have diabetes and an EF of 35% or less.
- Possible surgery or intervention as a treatment for coronary artery blockage, heart attack, valve disease (valve repair or replacement) or congenital heart disease.
Stage C treatment
The usual treatment plan for people with Stage C HF-rEF includes:
- Treatments listed in Stages A and B.
- Beta-blocker.
- Aldosterone antagonist if a vasodilator medicine (ACE-I, ARB or angiotensin receptor/neprilysin inhibitor combination) and beta-blocker don’t relieve your symptoms.
- Hydralazine/nitrate combination if other treatments don’t stop your symptoms. Patients who are Black should take this medication (even if they’re taking other vasodilator medications) if they have moderate to severe symptoms.
- Medications that slow your heart rate if your heart rate is faster than 70 beats per minute and you still have symptoms.
- A diuretic (“water pill”) may be prescribed if symptoms continue.
- Restriction of sodium (salt) in your diet.
- Tracking your weight every day. Tell your healthcare provider if you gain or lose more than four pounds.
- Possible fluid restriction.
- Possible cardiac resynchronization therapy (biventricular pacemaker).
- Possible implantable cardiac defibrillator (lCD) therapy.
If the treatment causes your symptoms to get better or stop, you still need to continue treatment to slow the progression to Stage D.
Stage D treatment
The usual treatment plan for people who have Stage D heart failure includes treatments listed in Stages A, B and C. In addition, it includes evaluation for more advanced treatment options, including:
- Heart transplant.
- Ventricular assist devices.
- Heart surgery.
- Continuous infusion of intravenous inotropic drugs.
- Palliative or hospice care.
- Research therapies.
Stages C and D with preserved EF
Treatment for people with Stage C and Stage D heart failure and preserved EF (HF-pEF) includes:
- Treatments listed in Stages A and B, although some may not be appropriate.
- Medications for the treatment of medical conditions that can cause heart failure or make the condition worse, such as atrial fibrillation, high blood pressure, diabetes, obesity, coronary artery disease, chronic lung disease, high cholesterol and kidney disease.
- Diuretic (“water pill”) to reduce or relieve symptoms.
It’s very important for you to manage your other health conditions, such as:
- Kidney disease.
- High blood pressure.
- Thyroid disease.
- Chronic lung disease.
Some conditions have signs and symptoms similar to heart failure. If you have new or worsening non-urgent symptoms, tell your healthcare provider.
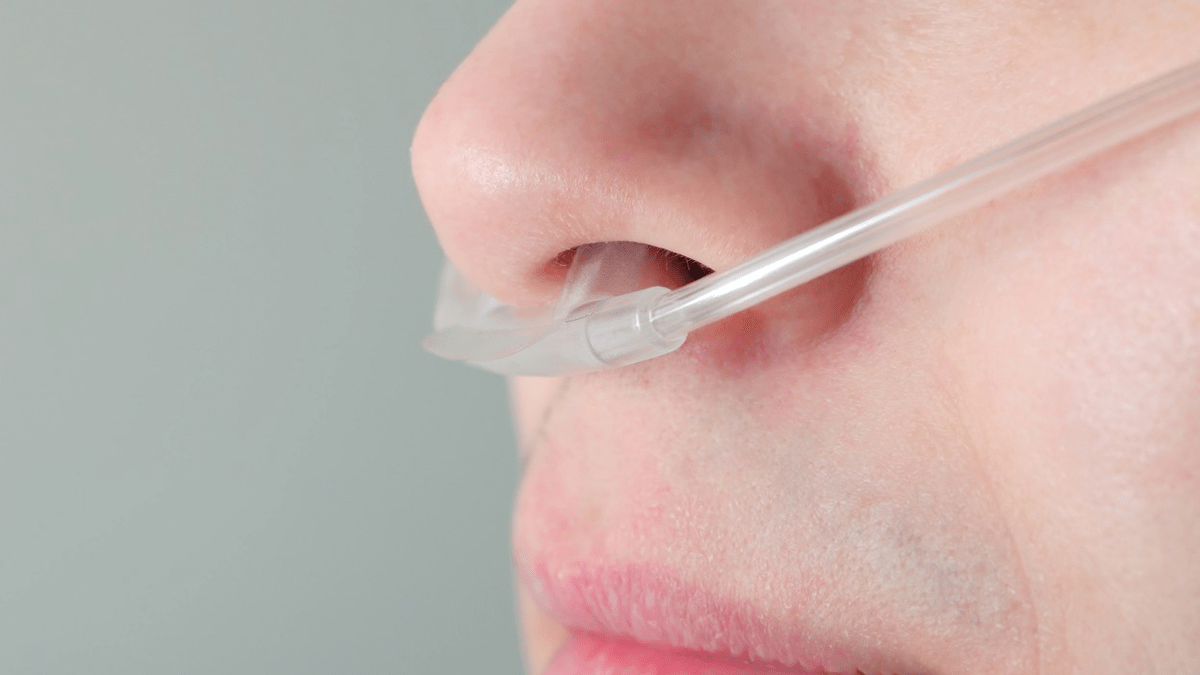
Oxygen Therapy with oxygen concentrator for Heart Failure
Oxygen therapy provides you with additional oxygen to ensure adequate oxygen supply for your body. It can be performed at home and is not a cure for heart failure, but it may prevent complications caused by low oxygen levels, such as heart and brain damage, as well as alleviate symptoms like breathlessness and ankle swelling. Your doctor usually recommends oxygen therapy when heart failure results in extremely low oxygen levels.
The basic idea is that you have a source of oxygen that you breathe in through either a:
- Mask that goes over your mouth and nose.
- Nasal cannula.
- Oxygen concentrator.
An oxygen concentrator may be the better choice, since constant tank refills can be costly and a hassle. This machine pulls oxygen directly from the air so you don’t need to worry about tanks or running out of oxygen. It does require electricity, so you’ll need a backup plan in case you lose power in your home or something goes wrong with the machine.
Contact us today to learn more about our services and how we can help you.
Heart failure and the effect on life quality and lifestyle
Many adults with heart failure are still able to live fulfilling lives with appropriate care and a well-designed treatment plan, despite some limitations in their activities. How well you feel depends on:
- How well your heart muscle is working.
- Your symptoms.
- How well you respond to your treatment plan.
- How well you follow your treatment plan.
This includes caring for yourself by:
- Taking your medications.
- Being active.
- Following a low-sodium diet.
- Tracking and reporting new or worsening symptoms to your provider.
- Keeping regular follow-up appointments with your healthcare provider.
Because heart failure is a chronic, long-term illness, talk to your doctor and your family about your preferences for medical care.